Published on July 3, 2024
There are more than one million limb amputations globally every year – that’s one every thirty seconds. Most are caused by peripheral vascular disease and diabetes, but there are also traumatic causes for an amputation.
Amputation of the leg – either above or below the knee – is the most common amputation surgery.

For people who need a lower-limb amputation, a well-fitting prosthesis is an important part of their successful rehabilitation. Restoring mobility allows amputees to access education and employment as well as enjoying family and social life.
But not everyone can access good prosthetics.
A simple, low-cost method for creating customised prosthetic sockets is now helping amputees in Indonesia.
Designed by Professor Peter Lee from the University of Melbourne, the pressure-casting (PCAST) system is being used to make prostheses in regions with limited resources and few trained prosthetists.

Sciences & Technology
A new leg to stand on
An estimated 80 per cent of the world’s disabled people live in low- or middle-income countries (LMICs), many of which have no prosthetics training programs and not enough trained prosthetists to meet demand. With so few prosthetics services in LMICs, many amputees have no access to limb-fitting facilities.
“Our work shows that you don’t need fancy equipment to make good prostheses,” says Professor Lee.
Challenges in traditional prosthetic fitting
The socket is the only part of an artificial limb that makes contact with the amputee’s remaining limb. So, it’s crucial to have a proper fit to allow for comfortable movement without pain.
The wrong fit can place too much pressure on sensitive parts of the residual limb or cause skin irritation and damage.

Making a commonly used socket, the patellar-tendon-bearing (PTB) socket, is time-consuming and labour-intensive.
First developed in the 1950s, the PTB socket was designed to distribute pressure to parts of the residual limb that were thought to be more pressure tolerant. But the PTB socket requires multiple fittings and modifications by a qualified prosthetist.
Recognising the need for a more accessible solution, Professor Lee and his team set out to develop a method that minimises the skills needed as well as reducing the time and cost of making a socket.
How the PCAST system works
The team’s PCAST system uses water pressure to shape the socket precisely to a person’s residual limb. Only basic materials are needed: a portable tank, water supply, plaster wrap and a weighing machine.
First, a plaster cast is applied over the residual limb. The person then uses their intact limb to stand on the weighing machine, while placing their residual limb into the tank.
Inside the tank, the residual limb is waterproofed by a plastic membrane. Water then fills the tank, and the person ensures that half their body weight is placed on the PCAST system.
The water applies uniform pressure on the plaster wrap, pressing it evenly around the residual limb.
After the plaster has hardened into the shape of the remaining limb, the water pressure is reduced.
A technician then makes a positive mould of the plaster cast (again, using plaster) and laminates it with resin or heated thermoplastic to create the final socket.
Studies show that PCAST sockets fit comfortably and compares well to PTB sockets in distributing pressure across the residual limb.
A focus on low- and middle-income countries
With a grant from the CASS Foundation, a private philanthropic organisation, Professor Lee aimed to study PCAST sockets further in Australia.
But a conversation with the foundation helped to change that focus.
Health & Medicine
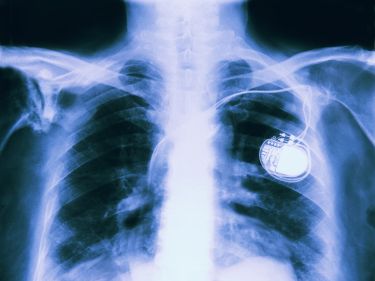
Part human, part robot: The future of medical implantables
“They pointed out that this technique will benefit people in places where there is a lack of skilled prosthetists and few facilities to fit artificial limbs,” says Professor Lee.
“They encouraged us to translate this research rather than just keeping it the lab. This was really a turning point for us.”
From the lab to the real world
With funding from the CASS Foundation and the Rotary Club of Richmond, the research team ran their first trial of the PCAST system in an LMIC, working in collaboration with VIETCOT, a training centre for orthopaedic technologists in Hanoi, Vietnam.
Many thousands of people have lost limbs to landmines in Vietnam, but traffic accidents, workplace injuries and diseases like diabetes also contribute to the prevalence of lower-limb amputations.

With help from the researchers, VIETCOT technicians created PCAST sockets for 32 volunteers, who used them regularly over five months.
“We were ready for it to be a total failure, but it was really eye-opening for us,” says Professor Lee. The volunteers reported high levels of satisfaction with the PCAST socket, and their performance in physical tests improved over time.
The research team also conducted another study at VIETCOT to compare PCAST sockets with PTB sockets in 17 volunteers. The researchers found no significant differences between the sockets in terms of the volunteers’ mobility, function, gait, comfort or socket preference.
Because the PCAST system is quicker and requires less skill than traditional socket-making techniques, it allows prosthetists to focus more time on amputees who have more complex needs.

Health & Medicine
Moving with the power of thought
Sharing the technology
To increase uptake of the technology in LMICs, Professor Lee is now focused on projects to upskill local practitioners in Indonesia and Tanzania.
In Indonesia, he is working with rehabilitation provider YAKKUM to teach technicians and clinicians how to use the PCAST system. The hope is that this approach, designed in collaboration with Associate Professor Noel Lythgo from RMIT University, will become a sustainable model that can be replicated.
“Using PCAST means that our prosthetics production is faster, more efficient and accurate,” says Rita Triharyani, the in-country project manager of YAKKUM’s Digital Health Hub Rehabilitation Program.
“The patient gets a socket with the same quality without waiting too long.”

YAKKUM technicians have made 133 PCAST sockets so far, including for people in remote areas who would otherwise have no access to limb-fitting facilities. The organisation conducts community visits so they “can bring the PCAST system to the field and do the casting process there”.
Based on the success of this project, Professor Lee is now working on a pilot project in Tanzania to make PCAST sockets for amputees in rural districts.
The 100 Limbs Project is a collaboration with the Global Peace Network, a Canadian NGO that uses distance education as part of its strategy to deliver rehabilitation in remote regions.
“In a country of more than 65 million people, there are only about 200 prosthetists in Tanzania and most of them work in big cities or private clinics,” says Dr Brian Budgell, president of the Global Peace Network.

Health & Medicine
Five ways 3D printing is changing medicine
As part of the project, they will train healthcare professionals how to use the PCAST system to create high-quality sockets.
“The PCAST system will allow us to add another dimension to our services and address a desperate need in the communities that we serve.”
Professor Lee is hopeful that widespread use of the PCAST system will provide more lower-limb amputees in LMICs with mobility and independence.
“When someone comes in on crutches and then walks out with a new leg – it’s almost like a miracle,” he says.
“It really transforms lives.”
This article was first published on Pursuit. Read the original article.