Published on August 13, 2024
There are over 30 trillion bacterial and fungal cells in the human microbiome. Most are harmless to us, their host, but some are not.
So how do the members of this vast microbial community get along with each other? And what happens when they don’t get along?
Bacteria and fungi are ‘frenemies’
Bacteria and fungi coexist in microbial communities in nearly all environments, from our bodies to the ocean depths.
In these microbial communities the interactions between bacteria and fungi can be both positive and negative. On the positive side we find synergisms, where the two groups of organisms support each other, like where there is a mutual sharing of nutrients.
But there can also be antagonism, where one is harmful to the other. In fact, many antibiotics that we use to kill bacteria originate from fungi.
The most famous example is penicillin which was originally found by accident when a spore of the fungus Penicillium accidentally landed on a petri dish that had been seeded with bacteria in the microbiology laboratory of St Mary’s hospital in London.

Health & Medicine
Is ‘herd immunity’ in intensive care doing more harm than good?
Antibiotics cause imbalance
Antibiotics will kill off certain types of bacteria, which can lead to an imbalance in our biome.
This imbalance can cause harm. For example, a simple course of antibiotics might result in a bout of diarrhoea.
With more prolonged antibiotic therapy, fungi and bacteria that are not susceptible to the antibiotic therapy can ‘overgrow’.
For example, many people will be familiar with one unpleasant side-effect of antibiotics – thrush. This occurs when the antibiotic triggers an overgrowth of the yeast fungus Candida, resulting in an outbreak of the yeast infection – typically in the vagina or mouth – we call thrush.
While thrush is relatively easy to treat, in more serious cases a microbiome imbalance can damage the gastrointestinal tract and result in invasion of new, harmful microbes.

Another example of imbalance that is a major problem for patients receiving antibiotic therapy in hospital is Clostridium difficile. Antibiotic-derived overgrowth of this bacteria can be a serious and life-threatening infection.
An increasingly common solution to correcting an imbalance caused by antibiotics is a transplant of faeces from healthy human donors. This faeces contains ‘healthy’ beneficial bacteria that can re-colonise the patient’s microbiome.
Faecal transplants are now an established intervention for at risk patients.

Sciences & Technology
Postbiotics: the new kid in the gut health family
Microbial interactions affect human health
With Candida overgrowth, it’s not just thrush, an infection limited to the mucosa (the nose, mouth and genitals), that we need to worry about.
Half of long-term ICU patients will be colonised with Candida and around 10 per cent will acquire an invasive Candida infection – a potentially fatal infection where the fungus gets into a patient’s bloodstream.
There is also laboratory evidence that suggests that interactions between Candida and other bacteria in the patient microbiome has the potential to promote invasive bacterial infections.
This has led to studies to explore whether the risk of bacterial pneumonia is increased in patients with Candida colonisation and whether antifungal treatments might reduce this likelihood.
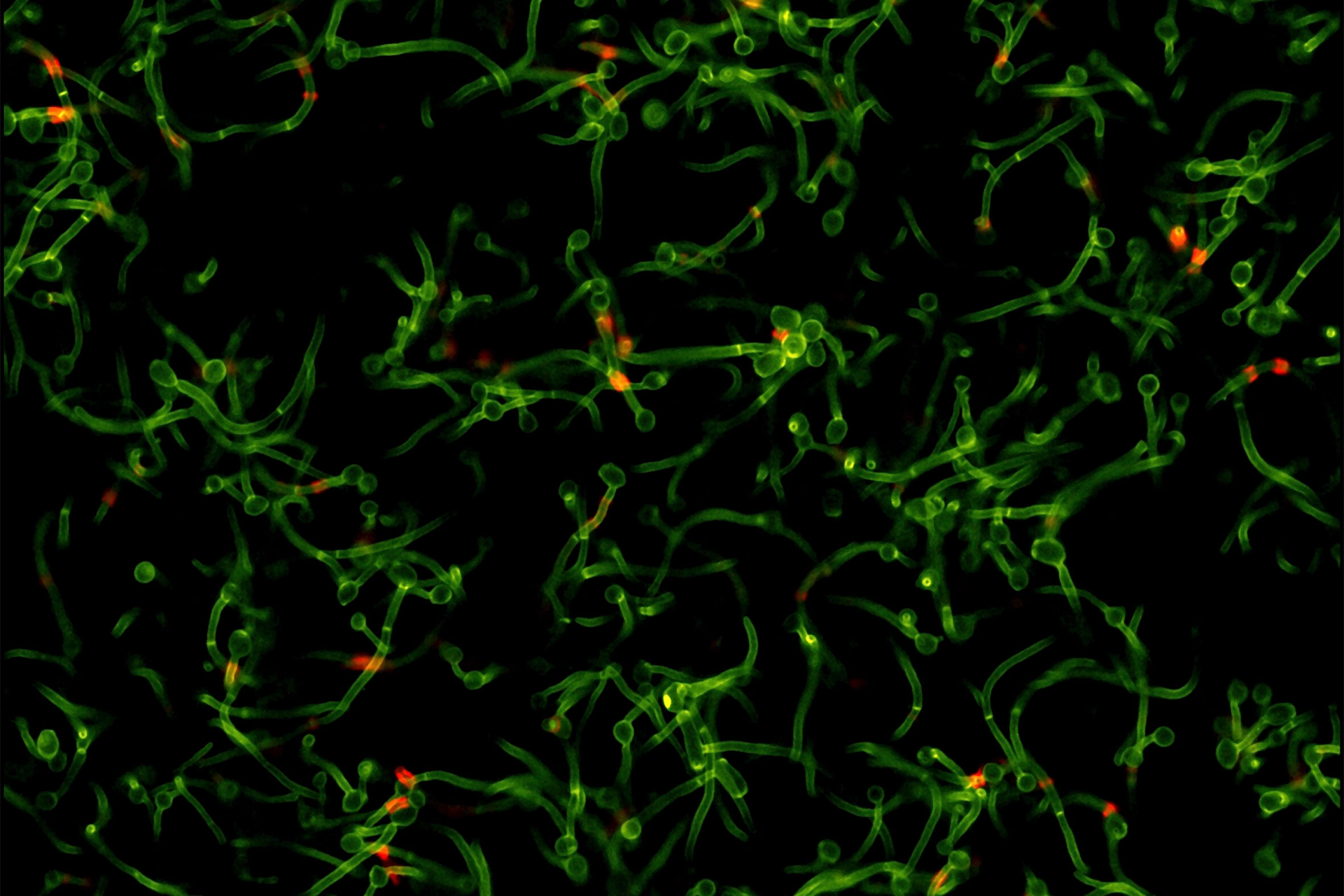
We want to understand why these microbial interactions occur. There are over 600 catalogued immunological, biochemical, metabolic and mechanical processes that could underlie the interaction between Candida and harmful bacteria like Pseudomonas aeruginosa.
But studying them in the human host is not simple. It is neither ethical nor practical to administer Candida to humans – especially to those in intensive care – to determine whether harmful bacterial infections might result.
What is the role of fungal-bacterial interactions in human critical illness?
To examine this question, I looked at data from over 300 published studies of antimicrobial treatments for preventing infections in patients in Intensive Care Units (ICU). These treatments target either Candida or bacteria or both.
Whilst the results of these studies are intriguing, the individual studies are somewhat small and inconclusive.
Collectively, however, these studies might allow us to answer questions like how might exposures to different antimicrobials drive otherwise unobservable microbial interactions?

Health & Medicine
Healthcare has a waste problem, but we can achieve net zero
Applying social science techniques to medical research
I have applied an analysis technique called Structural Equation Modelling (SEM) to the data from these studies. SEM is a technique for modelling potential causal links, and has a rich history in areas like psychology, ecology and econometrics.
But it hasn’t been used much in medicine.
SEM lets us estimate latent (unobservable) variables. For example, in social sciences SEM is used to explore relationships between difficult to observe variables like self-esteem, depression and social support under the influence of various ‘drivers’.
Hence, the technique is well suited to estimating the difficult to observe interactions between Candida and bacteria within the patient microbiome.
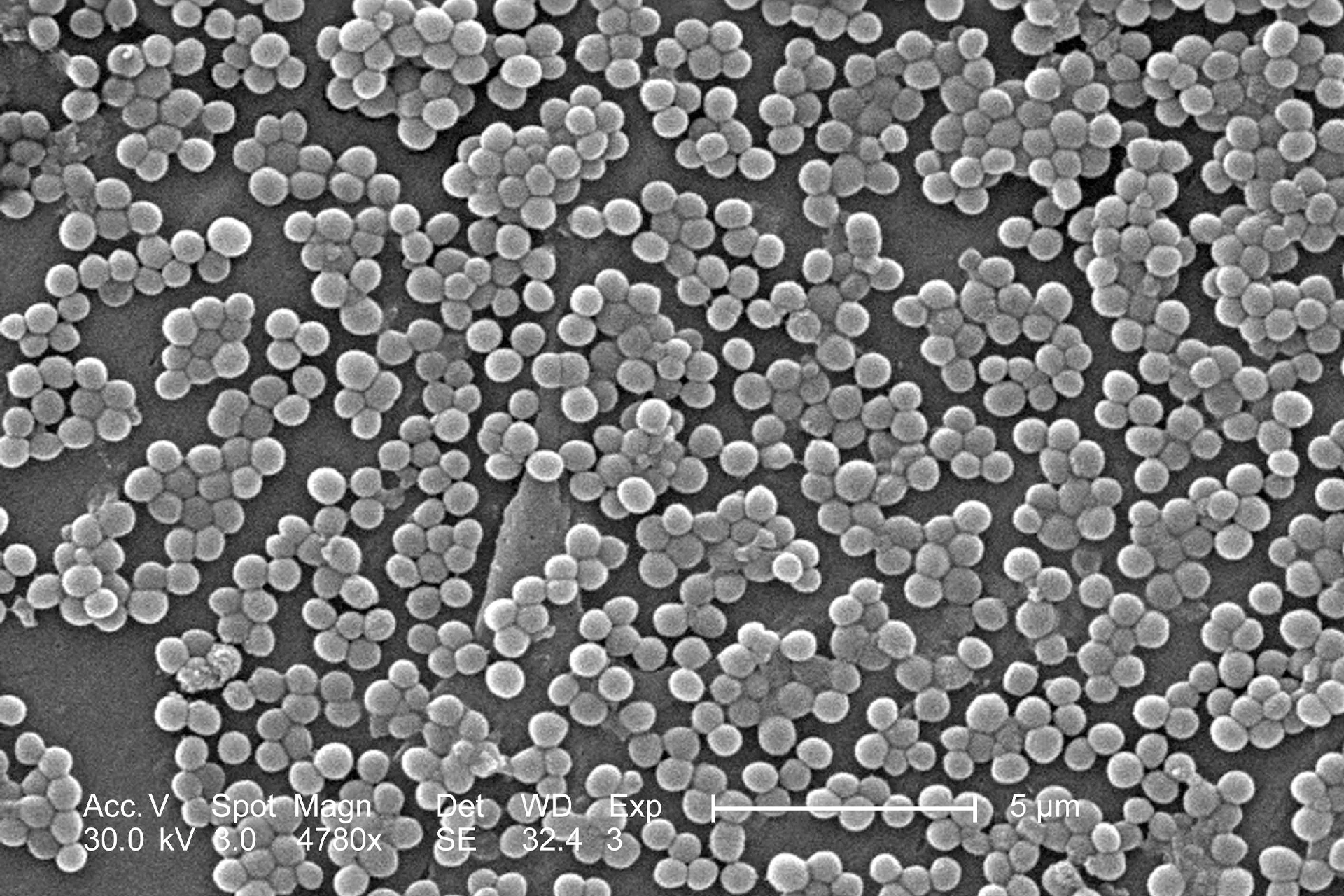
My SEM-based modelling has revealed that the anti-fungal agent amphotericin, when used as part of an antimicrobial prophylaxis regimen, can halve the incidence of Staphylococcus aureus blood stream infection (bacteraemia).
This is unexpected because amphotericin lacks activity against bacteria like Staphylococcus.
However, another anti-fungal agent, nystatin, does not offer the same protection against bacteraemia that amphotericin does.
My research found similar relationships between amphotericin and blood stream infections with other bacteria like Pseudomonas aeruginosa and Acinetobacter.

Health & Medicine
Ending the global tuberculosis epidemic
Blood stream infections with these specific bacteria are quite rare, so while amphotericin seems to halve the number infections, the absolute difference in incidence across all patients would be less than one percentage point.
This is a clinically significant reduction that would save lives, but the difference would be difficult to detect without SEM modelling.
SEM has a bright future in clinical research
SEM techniques offer great potential for clinical research on the microbiome and the impact of antimicrobials.
My research has established the usefulness of these techniques in the study of fungal-facilitated bacterial infections.
These methods will likely also enable us to use clinical data to test the activity of antimicrobial agents for a range of potential interactions, like with interactions with vitamins and other supplements.
This article was first published on Pursuit. Read the original article.